Updated at 5:53 p.m. on January 31, 2025
Last night, scientists began to hear cryptic and foreboding warnings from colleagues: Go to the CDC website, and download your data now. They were all telling one another the same thing: Data on the website were about to disappear, or be altered, to comply with the Trump administration’s ongoing attempt to scrub federal agencies of any mention of gender, DEI, and accessibility. “I was up until 2 a.m.,” Angela Rasmussen, a virologist at the Vaccine and Infectious Disease Organization at the University of Saskatchewan who relies on the CDC’s data to track viral outbreaks, told me. She archived whatever she could.
What they feared quickly came to pass. Already, content from the CDC’s Youth Risk Behavior Surveillance System, which includes data from a national survey, has disappeared; so have parts of the Agency for Toxic Substances and Disease Registry’s Social Vulnerability Index and the Environmental Justice Index. The CDC’s landing page for HIV data has also vanished. And the agency’s AtlasPlus tool, which contains nearly 20 years of CDC surveillance data on HIV, hepatitis, sexually transmitted infections, and tuberculosis, is down. Several scientists I talked with told me they had heard directly from contacts at the CDC that the agency has directed employees to scrub any mention of “gender” from its site and the data that it shares there, replacing it with “sex.”
The full scope of the purge isn’t yet clear. One document obtained by The Atlantic indicated that the government was, as of yesterday evening, intending to target and replace, at a minimum, several “suggested keywords”—including “pregnant people, transgender, binary, non-binary, gender, assigned at birth, binary [sic], non-binary [sic], cisgender, queer, gender identity, gender minority, anything with pronouns”—in CDC content. While these terms are often politicized, some represent demographic variables that researchers collect when tracking the ebb and flow of diseases and health conditions across populations. Should they be reworded, or even removed entirely, from data sets to comply with the executive order, researchers and health-care providers might have a much harder time figuring out how diseases affect specific communities—making it more challenging to serve Americans on the whole.
CDC data’s “explicit purpose” is to guide researchers toward the places and people who most need attention, Patrick Sullivan, an epidemiologist at Emory University and a former CDC Epidemic Intelligence Service officer, told me. As the changes unfold before him, he said, “it’s hard to understand how this benefits health.”
When I contacted the CDC, a spokesperson redirected my requests for comment to the Department of Health and Human Services. After this story was published, an HHS spokesperson said that “all changes to the HHS website and HHS division websites are in accordance with President Trump’s January 20 Executive Orders” on gender and DEI.
The government appears to understand that these changes could have scientific implications: The document directing a review of CDC content suggests that some work could be altered without “changing the meaning or scientific integrity of the content,” and that any such changes should be considered “routine.” Changing other content, according to the document, would require review by an expert precisely because any alterations would risk scientific integrity. But the document does not specify how data would be sorted into those categories, or at whose discretion.
“My fear is that in the short term, entire data sets would be taken down,” then reappear with demographic variables removed or altered to conform with DEI restrictions, Katie Biello, an epidemiologist at Brown, told me. Excising mention of gender and sexual orientation, for instance, from public-health data sets could require stripping entire columns of data out. If the government chooses to define sex as binary, transgender people and nonbinary people, among others, could be effectively erased. In response to the ongoing changes, some groups of researchers are now rushing to archive the CDC website in full.
Acknowledging and addressing health differences among demographic groups is a basic epidemiological tenet, Biello told me, “so we know where to target our health interventions.” She pointed to examples in her own field: Gay men have higher rates of STIs, but lower rates of obesity; transgender women have higher rates of HIV, but lower rates of prostate cancer. More broadly, demographic changes to data sets could limit the country’s ability to identify which Americans are most at risk from an expansive list of conditions including adolescent depression, STIs, even sex-specific cancers. Changing data sets in this way would be tantamount to “erasing our ability to use data and evidence” to care for people, Rachel Hardeman, a health-equity expert at the University of Minnesota, told me.
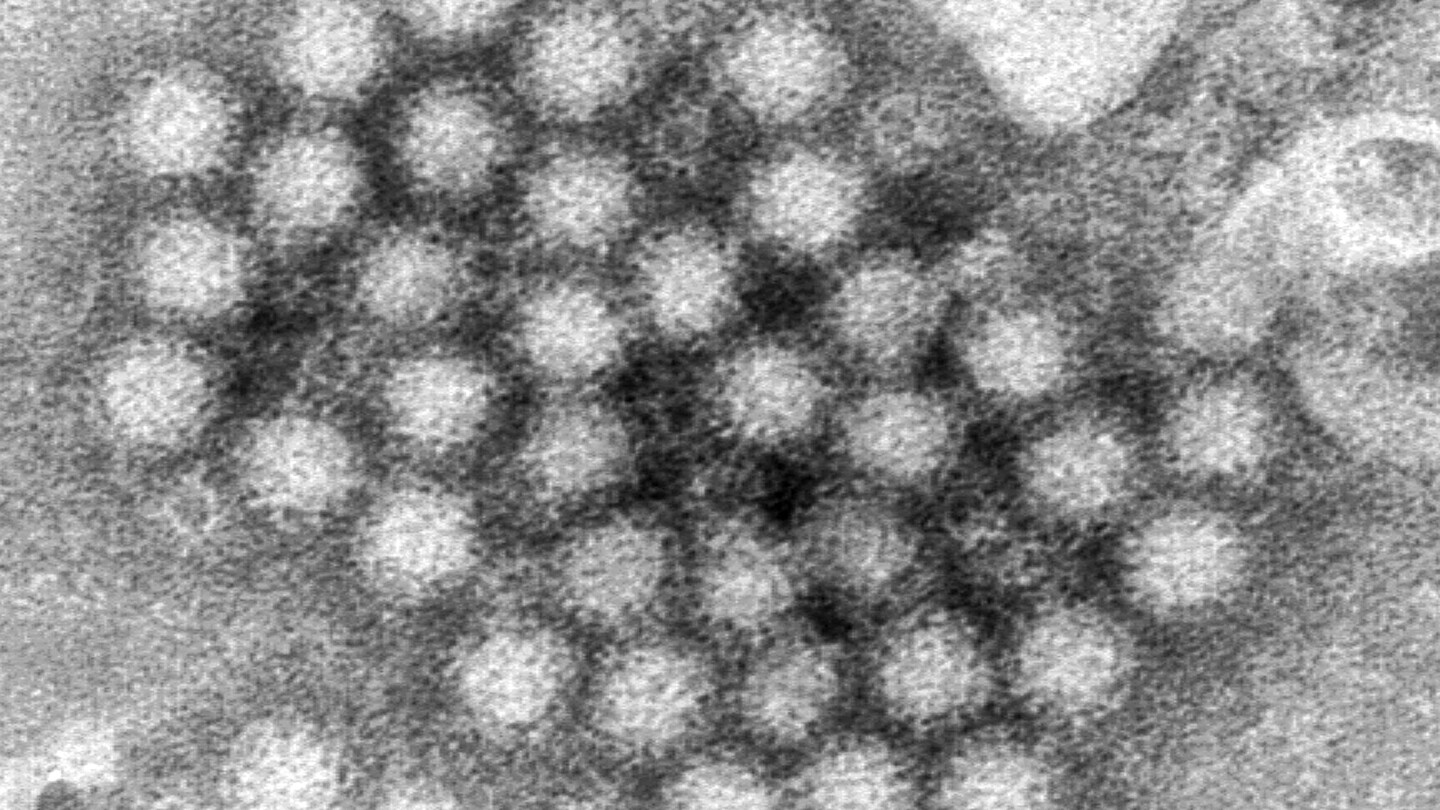
Jennifer Nuzzo, an epidemiologist at Brown, pointed to mpox as a recent example of how replacing “gender” with “sex,” or ignoring sexual orientation, could limit effective public-health responses. At the beginning of the United States’ 2022 outbreak, neither researchers nor the public had much clarity on who was most affected, leading to widespread panic. “Officials were talking about the situation as if it was a risk we equally faced,” Nuzzo said. By collecting detailed demographic information, researchers were able to show that the disease was primarily affecting men who have sex with men, allowing officials to more efficiently allocate resources, including vaccines, and bring the epidemic under control before it affected Americans more widely.
A scrub such as this could also change how the government allocates funds for long-standing threats to public health, which could widen health-equity gaps, or reverse progress in combatting them. Rates of STIs more generally have recently begun to plateau in the U.S., after decades of steady increase—but altering data that focus interventions on, say, transgender populations, or men who have sex with men, could undo those gains. If no data exist to prove that a health issue concentrates within a particular community, that “provides a justification to cut funding,” one researcher told me. (Several scientists who spoke with me for this article requested anonymity, for fear of retaliation for speaking out about the loss of federal data.) Sullivan, whose work focuses on HIV surveillance, compared the government’s actions to, effectively, destroying the road map to determining who in America most needs screening, pre-exposure prophylaxis, and treatment.
Much of the data on the CDC website have been aggregated from states, so it would be possible for researchers to reassemble those data sets, Nuzzo pointed out. But that’s an onerous task, and several scientists told me they never thought they’d be in a position where they’d have to scramble to squirrel away publicly available federal data. Nuzzo also worried that states might be reluctant in the future to share data with the federal government, or might decide not to bother collecting certain data at all. On the most basic scientific level, changing federal-government data means those data become unreliable. Public-health data are collected with the intention of sussing out which populations most need health interventions; altering those data leaves behind a skewed portrait of reality.
The Centers for Disease Control and Prevention (CDC) has come under scrutiny after reports surfaced that the agency is altering data to align with President Trump’s recent executive order banning critical race theory and diversity training in federal agencies.
The order, which aims to combat what the administration calls “divisive and anti-American propaganda,” has prompted concerns that the CDC is now censoring information related to race and inequality in public health data.
Critics argue that by altering data to fit the administration’s narrative, the CDC is compromising its integrity and undermining its mission to provide accurate and unbiased information to the public.
This move raises serious questions about the politicization of public health data and the potential impact on efforts to address systemic racism and health disparities in the United States.
It is crucial that the CDC remains independent and transparent in its data collection and reporting, and that any attempts to manipulate information for political purposes are met with swift condemnation and accountability.
The public health of our nation depends on the CDC’s ability to provide reliable and unbiased data, and any efforts to undermine this vital role must be met with resistance.
Tags:
- CDC data manipulation
- Trump DEI order impact on CDC
- CDC changing data for Trump
- Trump administration influence on CDC data
- CDC data accuracy under Trump
- CDC data integrity concerns
- Trump’s DEI order and CDC data alteration
- Political influence on CDC data
- CDC data transparency issues
- CDC data manipulation controversy
#CDC #Altering #Data #Follow #Trumps #DEI #Order