Your cart is currently empty!
Tag: Schizophrenia
A systematic review of passive data for remote monitoring in psychosis and schizophrenia
NHS. Psychosis. https://www.nhs.uk/mental-health/conditions/psychosis/overview/ (2023).
Almond, S., Knapp, M., Francois, C., Toumi, M. & Brugha, T. Relapse in schizophrenia: costs, clinical outcomes and quality of life. Br. J. Psychiatry 184, 346–351 (2004).
Lin, C., Zhang, X. & Jin, H. The societal cost of schizophrenia: an updated systematic review of cost-of-illness studies. PharmacoEconomics 41, 139–153 (2023).
Alvarez-Jimenez, M. et al. Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr. Res. 139, 116–128 (2012).
Ascher-Svanum, H. et al. The cost of relapse and the predictors of relapse in the treatment of schizophrenia. BMC Psychiatry 10, 7 (2010).
Phahladira, L. et al. Early recovery in the first 24 months of treatment in first-episode schizophrenia-spectrum disorders. npj Schizophrenia https://doi.org/10.1038/s41537-019-0091-y (2020).
Gleeson, J. F. et al. Systematic review of early warning signs of relapse and behavioural antecedents of symptom worsening in people living with schizophrenia spectrum disorders. Clin. Psychol. Rev. https://doi.org/10.1016/j.cpr.2023.102357 (2024).
Lewis, S. et al. Smartphone-enhanced symptom management in psychosis: open, randomized controlled trial. J. Med. Internet Res. 22, e17019 (2020).
Wee, Z. Y. et al. Actigraphy studies and clinical and biobehavioural correlates in schizophrenia: a systematic review. J. Neural Transmiss. 126, 531–558 (2019).
Trull, T. J. & Ebner-Priemer, U. Ambulatory assessment. Annu. Rev. Clin. Psychol. 9, 151–176 (2013).
Bucci, S., Schwannauer, M. & Berry, N. The digital revolution and its impact on mental health care. Psychol. Psychother. 92, 277–297 (2019).
Torous, J. et al. The growing field of digital psychiatry: current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry 20, 318–335 (2021).
Mohr, D. C., Zhang, M. & Schueller, S. M. Personal sensing: understanding mental health using ubiquitous sensors and machine learning. Annu. Rev. Clin. Psychol. 13, 23–47 (2017).
Renn, B. N., Pratap, A., Atkins, D. C., Mooney, S. D. & Areán, P. A. Smartphone-based passive assessment of mobility in depression: challenges and opportunities. Ment. Health Phys. Act. 14, 136–139 (2018).
Kiang, M. V. et al. Sociodemographic characteristics of missing data in digital phenotyping. Sci. Rep. https://doi.org/10.1038/s41598-021-94516-7 (2021).
Dixon, W. G. et al. Charting a course for smartphones and wearables to transform population health research. J. Med. Internet Res. 25, e42449 (2023).
Barnett, I., Torous, J., Staples, P., Keshavan, M. & Onnela, J.-P. Beyond smartphones and sensors: choosing appropriate statistical methods for the analysis of longitudinal data. J. Am. Med. Inform. Assoc. 25, 1669–1674 (2018).
Benoit, J., Onyeaka, H., Keshavan, M. & Torous, J. Systematic review of digital phenotyping and machine learning in psychosis spectrum illnesses. Harvard Rev. Psychiatry https://doi.org/10.1097/HRP.0000000000000268 (2020).
De Angel, V. et al. Digital health tools for the passive monitoring of depression: a systematic review of methods. npj Digital Med. https://doi.org/10.1038/s41746-021-00548-8 (2022).
Gomes, E. et al. Effects of a group physical activity program on physical fitness and quality of life in individuals with schizophrenia. Ment. Health Phys. Act. 7, 155–162 (2014).
Torous, J. et al. Characterizing the clinical relevance of digital phenotyping data quality with applications to a cohort with schizophrenia. NPJ Digital Med. 1, 15 (2018).
Afonso, P., Brissos, S., Figueira, M. L. & Paiva, T. Schizophrenia patients with predominantly positive symptoms have more disturbed sleep-wake cycles measured by actigraphy. Psychiatry Res. 189, 62–66 (2011).
Wulff, K., Dijk, D. J., Middleton, B., Foster, R. G. & Joyce, E. M. Sleep and circadian rhythm disruption in schizophrenia. Br. J. Psychiatry 200, 308–316 (2012).
Adler, D. A., Wang, F., Mohr, D. C. & Choudhury, T. Machine learning for passive mental health symptom prediction: Generalization across different longitudinal mobile sensing studies. PLoS ONE 17, e0266516 (2022).
Raugh, I. M. et al. Digital phenotyping adherence, feasibility, and tolerability in outpatients with schizophrenia. J. Psychiatr. Res. 138, 436–443 (2021).
Narkhede, S. M. et al. Machine learning identifies digital phenotyping measures most relevant to negative symptoms in psychotic disorders: implications for Clinical Trials. Schizophr. Bull. 48, 425–436 (2022).
Raugh, I. M. et al. Geolocation as a digital phenotyping measure of negative symptoms and functional outcome. Schizophr. Bull. https://doi.org/10.1093/schbul/sbaa121 (2020).
Fang, S.-H. et al. Associations between sleep quality and inflammatory markers in patients with schizophrenia. Psychiatry Res. 246, 154–160 (2016).
Deenik, J. et al. Changes in physical and psychiatric health after a multidisciplinary lifestyle enhancing treatment for inpatients with severe mental illness: The MULTI study I. Schizophr. Res. 204, 360–367 (2019).
Deenik, J., Tenback, D. E., Tak, E. C. P. M., Hendriksen, I. J. M. & van Harten, P. N. Improved psychosocial functioning and quality of life in inpatients with severe mental illness receiving a multidisciplinary lifestyle enhancing treatment. The MULTI study II. Ment. Health Phys. Act. 15, 145–152 (2018).
Browne, J. et al. Targeting physical health in schizophrenia: results from the Physical Activity Can Enhance Life (PACE-Life) 24-week open trial. Ment. Health Phys. Act. 20, 100393 (2021).
Mow, J. L. et al. Smartphone-based mobility metrics capture daily social motivation and behavior in schizophrenia. Schizophr. Res. 250, 13–21 (2022).
Thonon, B., Levaux, M.-N., van Aubel, E. & Laroi, F. A group intervention for motivational deficits: preliminary investigation of a blended care approach using ambulatory assessment. Behav. Modif. 46, 1167–1197 (2022).
Jongs, N. et al. A framework for assessing neuropsychiatric phenotypes by using smartphone-based location data. Transl. Psychiatry 10, 211 (2020).
Fowler, J. C. et al. Hummingbird study: results from an exploratory trial assessing the performance and acceptance of a digital medicine system in adults with schizophrenia, schizoaffective disorder, or first-episode psychosis. Neuropsychiatr. Dis. Treat. 17, 483–492 (2021).
Bueno-Antequera, J., Oviedo-Caro, M. A. & Munguia-Izquierdo, D. Ideal cardiovascular health and its association with sedentary behaviour and fitness in psychiatric patients. The PsychiActive project. Nutr., Metab. Cardiovasc. Dis. 28, 900–908 (2018).
Shamir, E. et al. Melatonin improves sleep quality of patients with chronic schizophrenia. J. Clin. Psychiatry 61, 373–377 (2000).
Depp, C. A. et al. GPS mobility as a digital biomarker of negative symptoms in schizophrenia: a case control study. npj Digital Med. 2, 108 (2019).
Henson, P., Pearson, J. F., Keshavan, M. & Torous, J. Impact of dynamic greenspace exposure on symptomatology in individuals with schizophrenia. PLoS ONE 15, e0238498 (2020).
Parrish, E. M. et al. Emotional determinants of life-space through GPS and ecological momentary assessment in schizophrenia: What gets people out of the house? Schizophr. Res. 224, 67–73 (2020).
Osipov, M., Behzadi, Y., Kane, J. M., Petrides, G. & Clifford, G. D. Objective identification and analysis of physiological and behavioral signs of schizophrenia. J. Ment. Health 24, 276–282 (2015).
Reinertsen, E. et al. Continuous assessment of schizophrenia using heart rate and accelerometer data. Physiol. Meas. 38, 1456–1471 (2017).
Reinertsen, E., Shashikumar, S. P., Shah, A. J., Nemati, S. & Clifford, G. D. Multiscale network dynamics between heart rate and locomotor activity are altered in schizophrenia. Physiol. Meas. 39, 115001 (2018).
Bengtsson, J., Olsson, E., Igelstrom, H., Persson, J. & Boden, R. Ambulatory heart rate variability in schizophrenia or depression: impact of anticholinergic burden and other factors. J. Clin. Psychopharmacol. 41, 121–128 (2021).
Strauss, G. P. et al. Validation of accelerometry as a digital phenotyping measure of negative symptoms in schizophrenia. Schizophrenia (Heidelb., Ger.) 8, 37 (2022).
Mayeli, A. et al. Shared and distinct abnormalities in sleep-wake patterns and their relationship with the negative symptoms of Schizophrenia Spectrum Disorder patients. Mol. Psychiatry https://doi.org/10.1038/s41380-023-02050-x (2023).
Dennison, C. A. et al. Association of genetic liability for psychiatric disorders with accelerometer-assessed physical activity in the UK Biobank. PLoS ONE 16, e0249189 (2021).
Ben-Zeev, D. et al. CrossCheck: integrating self-report, behavioral sensing, and smartphone use to identify digital indicators of psychotic relapse. Psychiatr. Rehabilit. J. 40, 266–275 (2017).
Buck, B. et al. Capturing behavioral indicators of persecutory ideation using mobile technology. J. Psychiatr. Res. 116, 112–117 (2019).
He-Yueya, J. et al. Assessing the relationship between routine and schizophrenia symptoms with passively sensed measures of behavioral stability. npj Schizophrenia 6, 35 (2020).
Barnett, I. et al. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology 43, 1660–1666 (2018).
Adler, D. A. et al. Predicting early warning signs of psychotic relapse from passive sensing data: an approach using encoder-decoder neural networks. JMIR mHealth uHealth 8, e19962 (2020).
Browne, J. et al. Virtual group-based walking intervention for persons with schizophrenia: a pilot randomized controlled trial. Ment. Health Phys. Act. 24, 100515 (2023).
Diamond, R. et al. The physical activity profiles of patients with persecutory delusions. Ment. Health Phys. Act. 23, 100462 (2022).
von Kanel, S. et al. Measuring catatonia motor behavior with objective instrumentation. Front. Psychiatry 13, 880747 (2022).
Zarbo, C. et al. Ecological monitoring of physical activity, emotions and daily life activities in schizophrenia: the DiAPAson study. BMJ Mental Health https://doi.org/10.1136/bmjment-2023-300836 (2023).
Holt, R. I. G. et al. Structured lifestyle education for people with schizophrenia, schizoaffective disorder and first-episode psychosis (STEPWISE): randomised controlled trial. Br. J. Psychiatry 214, 63–73 (2019).
Troiano, R. P. et al. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 40, 181–188 (2008).
Choi, L., Liu, Z., Matthews, C. E. & Buchowski, M. S. Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sports Exerc. 43, 357–364 (2011).
Martanto, W. et al. Association between wrist wearable digital markers and clinical status in Schizophrenia. Gen. Hosp. Psychiatry 70, 134–136 (2021).
Cohen, A. et al. Relapse prediction in schizophrenia with smartphone digital phenotyping during COVID-19: a prospective, three-site, two-country, longitudinal study. Schizophrenia 9, 6 (2023).
Lakhtakia, T. et al. Smartphone digital phenotyping, surveys, and cognitive assessments for global mental health: Initial data and clinical correlations from an international first episode psychosis study. Digital Health 8, 1–18 (2022).
Henson, P., Barnett, I., Keshavan, M. & Torous, J. Towards clinically actionable digital phenotyping targets in schizophrenia. npj Schizophrenia 6, 13 (2020).
Barnett, I. & Onnela, J. P. Inferring mobility measures from GPS traces with missing data. Biostatistics 21, e98–e112 (2020).
Brønd, J. C., Andersen, L. B. & Arvidsson, D. Generating ActiGraph counts from raw acceleration recorded by an alternative monitor. Med. Sci. Sports Exerc. 49, 2351–2360 (2017).
Bai, J. et al. An activity index for raw accelerometry data and its comparison with other activity metrics. PLoS ONE 11, e0160644 (2016).
Menghini, L., Cellini, N., Goldstone, A., Baker, F. C. & De Zambotti, M. A standardized framework for testing the performance of sleep-tracking technology: step-by-step guidelines and open-source code. Sleep https://doi.org/10.1093/sleep/zsaa170 (2021).
Cole, R. J., Kripke, D. F., Gruen, W., Mullaney, D. J. & Gillin, J. C. Automatic sleep/wake identification from wrist activity. Sleep 15, 461–469 (1992).
Rahimi-Eichi, H. et al. Open-source Longitudinal Sleep Analysis From Accelerometer Data (DPSleep): algorithm development and validation. JMIR mHealth uHealth 9, e29849 (2021).
Tan, Z.-H., Sarkar, A. K. & Dehak, N. rVAD: an unsupervised segment-based robust voice activity detection method. Comput. Speech Lang. 59, 1–21 (2020).
Migueles, J. H., Rowlands, A. V., Huber, F., Sabia, S. & Van Hees, V. T. GGIR: a research community–driven open source R package for generating physical activity and sleep outcomes from multi-day raw accelerometer data. J. Meas. Phys. Behav. 2, 188–196 (2019).
Blume, C., Santhi, N. & Schabus, M. ‘nparACT’ package for R: a free software tool for the non-parametric analysis of actigraphy data. MethodsX 3, 430–435 (2016).
Zlatintsi, A. et al. E-Prevention: Advanced Support System for Monitoring and Relapse Prevention in Patients with Psychotic Disorders Analyzing Long-Term Multimodal Data from Wearables and Video Captures. Sensors (Basel, Switzerland) https://doi.org/10.3390/s22197544 (2022).
Juda, M., Pater, J., Mistlberger, R. E. & Schutz, C. G. Sleep and rest-activity rhythms in recovering patients with severe concurrent mental and substance use disorder: a pilot study. J. Dual Diagn. 19, 26–39 (2023).
Bromundt, V. et al. Sleep – wake cycles and cognitive functioning in schizophrenia. Br. J. Psychiatry 198, 269–276 (2011).
Fasmer, E. E., Fasmer, O. B., Berle, J. O., Oedegaard, K. J. & Hauge, E. R. Graph theory applied to the analysis of motor activity in patients with schizophrenia and depression. PLoS ONE 13, e0194791 (2018).
Kas, M. J. H. et al. Digital behavioural signatures reveal trans-diagnostic clusters of Schizophrenia and Alzheimer’s disease patients: Trans-diagnostic clustering of digital biotypes. Eur. Neuropsychopharmacol. 78, 3–12 (2024).
Kalisperakis, E. et al. Smartwatch digital phenotypes predict positive and negative symptom variation in a longitudinal monitoring study of patients with psychotic disorders. Front. Psychiatry 14, 1024965 (2023).
Skeldon, A. C., Dijk, D.-J., Meyer, N. & Wulff, K. Extracting circadian and sleep parameters from longitudinal data in schizophrenia for the design of pragmatic light interventions. Schizophr. Bull. 48, 447–456 (2022).
Kuula, L., Halonen, R., Lipsanen, J. & Pesonen, A.-K. Adolescent circadian patterns link with psychiatric problems: a multimodal approach. J. Psychiatr. Res. 150, 219–226 (2022).
Pieters, L. E., Deenik, J., Tenback, D. E., Oort, J. V. & Harten, P. N. V. Exploring the relationship between movement disorders and physical activity in patients with schizophrenia: an actigraphy study. Schizophr. Bull. 47, 906–914 (2021).
Liebenthal, E. et al. Linguistic and non-linguistic markers of disorganization in psychotic illness. Schizophr. Res. https://doi.org/10.1016/j.schres.2022.12.003 (2022).
Mandel, F., Ghosh, R. P. & Barnett, I. Neural networks for clustered and longitudinal data using mixed effects models. Biometrics https://doi.org/10.1111/biom.13615 (2021).
Kay, S. R., Fiszbein, A. & Opler, L. A. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Cella, M. et al. Evaluating the mechanisms of social cognition intervention in schizophrenia: a proof-of-concept trial. Psychiatry Res. 319, 114963 (2022).
Orleans-Pobee, M. et al. Physical Activity Can Enhance Life (PACE-Life): results from a 10-week walking intervention for individuals with schizophrenia spectrum disorders. J. Ment. Health 31, 357–365 (2022).
Buck, B. et al. Relationships between smartphone social behavior and relapse in schizophrenia: a preliminary report. Schizophr. Res. 208, 167–172 (2019).
Walther, S., Ramseyer, F., Horn, H., Strik, W. & Tschacher, W. Less structured movement patterns predict severity of positive syndrome, excitement, and disorganization. Schizophr. Bull. 40, 585–591 (2014).
Lamichhane, B., Zhou, J. & Sano, A. Psychotic relapse prediction in schizophrenia patients using a personalized mobile sensing-based supervised deep learning model. IEEE J. Biomed. Health Inform. 10.1109/JBHI.2023.3265684 (2023).
Nguyen, D.-K., Chan, C.-L., Li, A.-H. A., Phan, D.-V. & Lan, C.-H. Decision support system for the differentiation of schizophrenia and mood disorders using multiple deep learning models on wearable devices data. Health Inform. J. 28, 14604582221137537 (2022).
Price, G. D. et al. An unsupervised machine learning approach using passive movement data to understand depression and schizophrenia. J. Affect. Disord. 316, 132–139 (2022).
Lahti, A. C., Wang, D., Pei, H., Baker, S. & Narayan, V. A. Clinical utility of wearable sensors and patient-reported surveys in patients with schizophrenia: noninterventional, observational study. JMIR Ment. Health 8, e26234 (2021).
Rohani, D. A., Faurholt-Jepsen, M., Kessing, L. V. & Bardram, J. E. Correlations between objective behavioral features collected from mobile and wearable devices and depressive mood symptoms in patients with affective disorders: systematic review. JMIR Mhealth Uhealth 6, e165 (2018).
Bayoumy, K. et al. Smart wearable devices in cardiovascular care: where we are and how to move forward. Nat. Rev. Cardiol. 18, 581–599 (2021).
Stradford, L. et al. Wearable activity tracker study exploring rheumatoid arthritis patients’ disease activity using patient-reported outcome measures, clinical measures, and biometric sensor data (the wear study). Contemp. Clin. Trials Commun. 38, 101272 (2024).
Jakobsen, P. et al. in 2020 IEEE 33rd International Symposium on Computer-Based Medical Systems (CBMS). (IEEE).
Asgari Mehrabadi, M. et al. Sleep tracking of a commercially available smart ring and smartwatch against medical-grade actigraphy in everyday settings: instrument validation study. JMIR Mhealth Uhealth 8, e20465 (2020).
Allan, S. et al. Adverse events reporting in digital interventions evaluations for psychosis: a systematic literature search and individual level content analysis of adverse event reports. Schizophr. Bull. https://doi.org/10.1093/schbul/sbae031 (2024).
Eisner, E. et al. Measurement of adverse events in studies of digital health interventions for psychosis: guidance and recommendations based on a literature search and framework analysis of standard operating procedures. Schizophr. Bull. https://doi.org/10.1093/schbul/sbae048 (2024).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. https://doi.org/10.1136/bmj.n71 (2021).
Steyerberg, E. W. et al. Prognosis Research Strategy (PROGRESS) 3: prognostic model research. PLoS Med. https://doi.org/10.1371/journal.pmed.1001381 (2013).
Riley, R. D. et al. Prognosis Research Strategy (PROGRESS) 2: prognostic factor research. PLoS Med. 10, e1001380–e1001380 (2013).
Hayden, J. A., van der Windt, D. A., Cartwright, J. L., Côté, P. & Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 158, 280–286 (2013).
Wolff, R. F. et al. PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann. Intern. Med. 170, 51–58 (2019).
Savage, C. L. G., Orth, R. D., Jacome, A. M., Bennett, M. E. & Blanchard, J. J. Assessing the psychometric properties of the PROMIS sleep measures in persons with psychosis. Sleep https://doi.org/10.1093/sleep/zsab140 (2021).
Reeve, S., Sheaves, B. & Freeman, D. Sleep disorders in early psychosis: incidence, severity, and association with clinical symptoms. Schizophr. Bull. 45, 287–295 (2019).
Baandrup, L. & Jennum, P. J. A validation of wrist actigraphy against polysomnography in patients with schizophrenia or bipolar disorder. Neuropsychiatr. Dis. Treat. 11, 2271–2277 (2015).
Walther, S., Horn, H., Koschorke, P., Muller, T. J. & Strik, W. Increased motor activity in cycloid psychosis compared to schizophrenia. World J. Biol. Psychiatry 10, 746–751 (2009).
Walther, S., Koschorke, P., Horn, H. & Strik, W. Objectively measured motor activity in schizophrenia challenges the validity of expert ratings. Psychiatry Res. 169, 187–190 (2009).
Walther, S. et al. Higher motor activity in schizophrenia patients treated with olanzapine versus risperidone. J. Clin. Psychopharmacol. 30, 181–184 (2010).
Wichniak, A. et al. Actigraphic monitoring of activity and rest in schizophrenic patients treated with olanzapine or risperidone. J. Psychiatr. Res. 45, 1381–1386 (2011).
Wang, J. et al. Both physical activity and food intake are associated with metabolic risks in patients with schizophrenia. Schizophr. Res. 140, 260–261 (2012).
Abel, D. B., Salyers, M. P., Wu, W., Monette, M. A. & Minor, K. S. Quality versus quantity: determining real-world social functioning deficits in schizophrenia. Psychiatry Res. 301, 113980 (2021).
Abel, D. B. & Minor, K. S. Social functioning in schizophrenia: comparing laboratory-based assessment with real-world measures. J. Psychiatr. Res. 138, 500–506 (2021).
Abplanalp, S. J. et al. Feasibility of using smartphones to capture speech during social interactions in schizophrenia. Schizophr. Res. 228, 51–52 (2021).
Reinertsen, E. & Clifford, G. D. A review of physiological and behavioral monitoring with digital sensors for neuropsychiatric illnesses. Physiol. Meas. 39, 05TR01 (2018).
Wainberg, M. et al. Association of accelerometer-derived sleep measures with lifetime psychiatric diagnoses: a cross-sectional study of 89,205 participants from the UK Biobank. PLoS Med. 18, e1003782 (2021).
Firth, J. et al. The validity and value of self-reported physical activity and accelerometry in people with schizophrenia: a population-scale study of the UK biobank. Schizophr. Bull. 44, 1293–1300 (2018).
Deenik, J. et al. Physical activity and quality of life in long-term hospitalized patients with severe mental illness: A cross-sectional study. BMC Psychiatry 17, 298 (2017).
Smit, M. M. C., Waal, E. D., Tenback, D. E. & Deenik, J. Evaluating the implementation of a multidisciplinary lifestyle intervention for people with severe mental illness in sheltered housing: effectiveness-implementation hybrid randomised controlled trial. BJPsych Open 8, e201 (2022).
Kruisdijk, F. et al. Accelerometer-measured sedentary behaviour and physical activity of inpatients with severe mental illness. Psychiatry Res. 254, 67–74 (2017).
Gomes, E. et al. Quality of life and physical activity levels in outpatients with schizophrenia. Rev. Bras. Psiquiatr. 38, 157–160 (2016).
Andersen, E. et al. Physical activity pattern and cardiorespiratory fitness in individuals with schizophrenia compared with a population-based sample. Schizophr. Res. 201, 98–104 (2018).
Andersen, E. et al. Effect of high-intensity interval training on cardiorespiratory fitness, physical activity and body composition in people with schizophrenia: a randomized controlled trial. BMC Psychiatry 20, 425 (2020).
Engh, J. A. et al. Objectively assessed daily steps-not light intensity physical activity, moderate-to-vigorous physical activity and sedentary time-is associated with cardiorespiratory fitness in patients with schizophrenia. Front. Psychiatry 10, 82 (2019).
Holmen, T. L. et al. The association between cardiorespiratory fitness and cognition appears neither related to current physical activity nor mediated by brain-derived neurotrophic factor in a sample of outpatients with schizophrenia. Front. Psychiatry 10, 785 (2019).
Janney, C. A. et al. Sedentary behavior and psychiatric symptoms in overweight and obese adults with schizophrenia and schizoaffective disorders (WAIST Study). Schizophr. Res. 145, 63–68 (2013).
Janney, C. A. et al. Physical activity and sedentary behavior measured objectively and subjectively in overweight and obese adults with schizophrenia or schizoaffective disorders. J. Clin. Psychiatry 76, e1277–e1284 (2015).
Lindamer, L. A. et al. Assessment of physical activity in middle-aged and older adults with schizophrenia. Schizophr. Res. 104, 294–301 (2008).
Duncan, M. J., Arbour-Nicitopoulos, K., Subramaniapillai, M., Remington, G. & Faulkner, G. Revisiting the International Physical Activity Questionnaire (IPAQ): assessing sitting time among individuals with schizophrenia. Psychiatry Res. 271, 311–318 (2019).
Berry, A., Drake, R. J., Butcher, I. & Yung, A. R. Examining the feasibility, acceptability, validity and reliability of physical activity, sedentary behaviour and sleep measures in people with schizophrenia. Ment. Health Phys. Act. 21, 100415 (2021).
Brobakken, M. F. et al. A comprehensive cardiovascular disease risk profile in patients with schizophrenia. Scand. J. Med. Sci. Sports 29, 575–585 (2019).
Jerome, G. J. et al. Physical activity levels of persons with mental illness attending psychiatric rehabilitation programs. Schizophr. Res. 108, 252–257 (2009).
Duncan, M. J., Arbour-Nicitopoulos, K., Subramanieapillai, M., Remington, G. & Faulkner, G. Revisiting the International Physical Activity Questionnaire (IPAQ): Assessing physical activity among individuals with schizophrenia. Schizophr. Res. 179, 2–7 (2017).
Gorczynski, P., Faulkner, G., Cohn, T. & Remington, G. Examining the efficacy and feasibility of exercise counseling in individuals with schizophrenia: a single-case experimental study. Ment. Health Phys. Act. 7, 191–197 (2014).
Gorczynski, P., Faulkner, G., Cohn, T. & Remington, G. Examining strategies to improve accelerometer compliance for individuals living with schizophrenia. Psychiatr. Rehabilit. J. 37, 333–335 (2014).
Grassmann, V., Subramaniapillai, M., Duncan, M., Arbour-Nicitopoulos, K. & Faulkner, G. E. The relationship between moderate-to-vigorous physical activity and executive function among individuals with schizophrenia: differences by illness duration. Rev. Bras. Psiquiatr. 39, 309–315 (2017).
Oliva, V. et al. Patterns of antipsychotic prescription and accelerometer-based physical activity levels in people with schizophrenia spectrum disorders: a multicenter, prospective study. Int. Clin. Psychopharmacol. 38, 28–39 (2023).
Chen, L. J., Steptoe, A., Chung, M. S. & Ku, P. W. Association between actigraphy-derived physical activity and cognitive performance in patients with schizophrenia. Psychol. Med. 46, 2375–2384 (2016).
Faulkner, G., Cohn, T. & Remington, G. Validation of a physical activity assessment tool for individuals with schizophrenia. Schizophr. Res. 82, 225–231 (2006).
Bueno-Antequera, J., Oviedo-Caro, M. & Munguia-Izquierdo, D. Sedentary behaviour, physical activity, cardiorespiratory fitness and cardiometabolic risk in psychosis: the PsychiActive project. Schizophr. Res. 195, 142–148 (2018).
Afonso, P., Figueira, M. L. & Paiva, T. Sleep-wake patterns in schizophrenia patients compared to healthy controls. World J. Biol. Psychiatry 15, 517–524 (2014).
Walther, S. et al. Quantitative motor activity differentiates schizophrenia subtypes. Neuropsychobiology 60, 80–86 (2009).
Beebe, L. H. et al. A pilot study describing physical activity in persons with schizophrenia spectrum disorders (Ssds) after an exercise program. Issues Ment. Health Nurs. 34, 214–219 (2013).
Williams, J. et al. ‘Walk this way’: results from a pilot randomised controlled trial of a health coaching intervention to reduce sedentary behaviour and increase physical activity in people with serious mental illness. BMC Psychiatry 19, 287 (2019).
Scheewe, T. W. et al. Low physical activity and cardiorespiratory fitness in people with schizophrenia: a comparison with matched healthy controls and associations with mental and physical health. Front. Psychiatry 10, 87 (2019).
Vancampfort, D. et al. Lower cardiorespiratory fitness is associated with more time spent sedentary in first episode psychosis: a pilot study. Psychiatry Res. 253, 13–17 (2017).
Vancampfort, D. et al. Validity and correlates of the International Physical Activity Questionnaire in first-episode psychosis. Early Interv. Psychiatry 13, 562–567 (2019).
Cella, M. et al. Using wearable technology to detect the autonomic signature of illness severity in schizophrenia. Schizophr. Res. 195, 537–542 (2018).
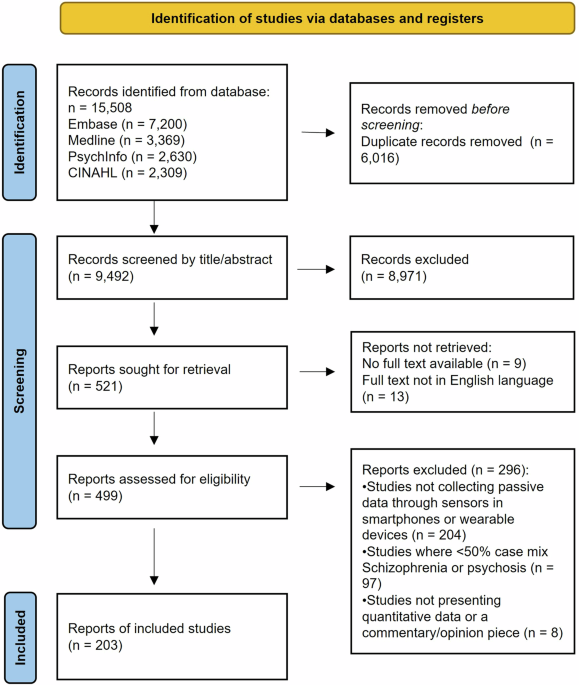
Passive data collection methods are increasingly being used in the field of mental health to remotely monitor symptoms and behaviors of individuals with psychosis and schizophrenia. In this post, we will conduct a systematic review of the current literature on the use of passive data for remote monitoring in these populations.Passive data collection refers to the continuous and unobtrusive monitoring of individuals using sensors and other technology to gather information about their daily activities, movements, and interactions. This data can provide valuable insights into the progression of symptoms, medication adherence, and overall well-being of individuals with psychosis and schizophrenia.
Several studies have explored the use of passive data collection methods such as smartphone sensors, wearable devices, and smart home technology to monitor symptoms and behaviors in individuals with psychosis and schizophrenia. These studies have shown promising results in terms of early detection of relapse, predicting hospitalizations, and improving outcomes through personalized interventions.
However, challenges remain in terms of privacy concerns, data security, and the integration of passive data into existing clinical workflows. Additional research is needed to further validate the effectiveness of passive data for remote monitoring in psychosis and schizophrenia, as well as to explore the potential barriers and facilitators to its implementation in clinical practice.
Overall, the use of passive data for remote monitoring in psychosis and schizophrenia holds great promise for improving the care and outcomes of individuals with these conditions. By conducting a systematic review of the current literature, we can better understand the current state of research in this area and identify key areas for future investigation and implementation.
Tags:
- Passive data monitoring
- Remote monitoring in psychosis
- Schizophrenia research
- Systematic review of passive data
- Mental health monitoring
- Remote sensing technology
- Psychosis and schizophrenia studies
- Data collection in mental health
- Wearable technology in mental health
- Remote patient monitoring
#systematic #review #passive #data #remote #monitoring #psychosis #schizophrenia

‘Star Wars’ Actor Jake Lloyd, 35, Shares Update on His Schizophrenia Journey
Jake Lloyd, the former child actor who played Anakin Skywalker in Star Wars: Episode I – The Phantom Menace, feels “pretty good” at the start of 2025.
Lloyd, now 35, recently completed an 18-month stay at an inpatient mental health facility in Southern California, author Clayton Sandell reported on Wednesday, Jan. 1. The actor, who was diagnosed with schizophrenia, is starting the new year living at a rehabilitation center where he is receiving treatment.
Lloyd’s mother Lisa Lloyd told Sandell her son struggled with anosognosia, which is common for those with schizophrenia. It is a condition “where your brain can’t recognize one or more other health conditions you have,” per the Cleveland Clinic, which adds that people with it are “much more likely to avoid or resist treatment for their other health conditions.”
Jake Lloyd ans his mother Lisa Lloyd in May 1999.
Ron Galella, Ltd./Ron Galella Collection via Getty
Never miss a story — sign up for PEOPLE’s free daily newsletter to stay up-to-date on the best of what PEOPLE has to offer, from celebrity news to compelling human interest stories.
When Sandell asked how he was doing, Lloyd had positive news to share.
“Pretty good, considering these 20 years of time that have come to an end,” Lloyd said. “I can now accept taking on continued treatment, and therapy, and my meds. Everyone’s been very supportive.” (Lisa later told Sandell it hasn’t been 20 years since he was diagnosed.)
Lloyd was 8 years old when George Lucas cast him as Anakin in The Phantom Menace, which meant his face was everywhere in 1999. Lisa told Sandell last year in an interview published by Scripps News that the negative response to the movie had nothing to do with his decision to leave acting behind or his mental health decline. She noted that there was a history of schizophrenia in his father’s family.
In 2015, Lloyd was arrested in South Carolina during a road trip from Florida to Canada. He spent 10 months in prison, which led to Lisa telling TMZ her son was diagnosed with schizophrenia. In May 2023, Lloyd had a complete “psychotic break” and was arrested after turning his car off in the middle of a three-lane road.
Hitting “rock bottom” was necessary to “honestly take part in treatment, honestly take your meds, and honestly live with your diagnosis,” Lloyd told Sandell.
Jake Lloyd in 2011.
Gilbert Carrasquillo/FilmMagic
The PEOPLE Puzzler crossword is here! How quickly can you solve it? Play now!
Today, Lloyd is a Star Wars fan himself and is playing through the franchise’s classic video games. Although he is not appearing at fan conventions, he told Sandell that the experiences he has had with fans are “immediately therapeutic.”
“I really do appreciate the time that’s been taken on us,” Lloyd said. “I’m very appreciative.”
Lloyd still has some catching up to do when it comes to Disney’s latest Star Wars projects. He told Sandell he was “holding out” for May the Fourth to watch as much as he can.
“Jake’s actually getting so much better than he was,” Lisa also told Sandell. “It’s a big relief for me and the rest of his family. We’re all just thrilled that he’s doing as well as he is, and that he’s working really hard at it. We appreciate that.”
If you or someone you know needs mental health help, text “STRENGTH” to the Crisis Text Line at 741-741 to be connected to a certified crisis counselor.
In a recent interview with People magazine, “Star Wars” actor Jake Lloyd opened up about his ongoing battle with schizophrenia.The 35-year-old actor, who is best known for his role as young Anakin Skywalker in “Star Wars: Episode I – The Phantom Menace,” revealed that he was diagnosed with schizophrenia in his late teens. Since then, he has been on a journey of self-discovery and healing.
Lloyd shared that living with schizophrenia has been a challenging and isolating experience, but he has found strength in therapy, medication, and the support of his loved ones. He emphasized the importance of seeking help and breaking the stigma surrounding mental illness.
Despite the obstacles he faces, Lloyd remains hopeful and determined to continue his journey towards recovery. He expressed gratitude for the love and encouragement he has received from fans and the “Star Wars” community.
Fans were quick to show their support for Lloyd, sending messages of love and encouragement on social media. Many praised his bravery in sharing his story and applauded his commitment to raising awareness about mental health issues.
We wish Jake Lloyd all the best on his journey and commend him for his courage in speaking out about his struggles. May the Force be with him as he continues to navigate his path towards healing and well-being.
Tags:
Star Wars, Jake Lloyd, schizophrenia journey, mental health, actor update, Hollywood news, mental illness awareness
#Star #Wars #Actor #Jake #Lloyd #Shares #Update #Schizophrenia #Journey
